Announcing bad news
Conveying a diagnosis or prognosis to family members requires great tact and compassion, as it needs to be done in circumstances that are always difficult and often sudden. Comforting and helping a grieving family faced with the expected or unexpected death of a loved one is never easy.
After being given the bad news, families are most often in a state of shock. Their ability to listen and analyze is affected significantly. This reality therefore needs to be considered when the time comes to inform them of a severe prognosis and its implications.
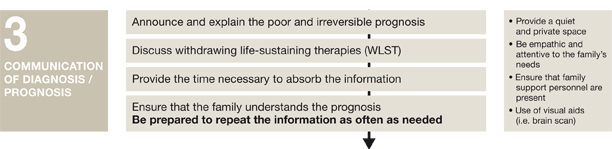
Best approach to communication
The decoupling approach is the best practice when it comes to speaking with the family. It is made up of three steps.
Step one:
The severe and irreversible prognosis is announced by the attending physician. For health centres with dedicated personnel, the nurse consultant in organ donation and care partnerships/resource nurse should ideally be present in order to continue supporting the family and respond, in conjunction with the treatment team, to any questions that follow about the organ donation process.
All discussions of this nature must take place in a setting that is conducive to supporting the families. The ideal environment is a quiet, private area. Keep an empathetic attitude, be attentive to their concerns and answer their questions with an eye to making it easier for them to make a free and informed decision. Back up explanations with visuals and medical imagery. All these recognized methods will make it easier to approach grieving families and support them most effectively.
Step two:
It is important to give families the time they need to understand the prognosis and its implications.
Step three:
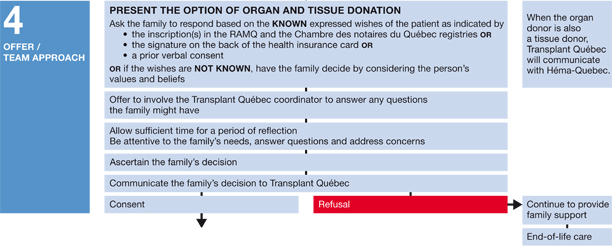
A - Proposing the organ donation option/known wishes
Once it has been established that the family understands the diagnosis or the severe and irreversible prognosis, the organ donation option can be broached with the family by asking them to respond based on their knowledge of the deceased patient’s expressed wishes.
At this point it becomes imperative to know the potential donor’s wishes regarding organ and tissue donation.
To find out, as stipulated in article 204.1 of the Act Respecting Health Services and Social Services (RSQ, c S-4.2), your institution’s nurse consultant in organ donation and care partnerships/resource nurse must contact Transplant
Québec to verify whether the patient is listed in Quebec’s consent registries:
- The RAMQ organ and tissue donation consent registry
- The organ and tissue donor consent registry established by the Chambre des notaires du Québec
The information in these registries is crucial to helping the family honour the wishes of their loved one.
In addition to verifying these consent registries, check whether the potential donor had signed the consent sticker on the back of his or her health insurance card, as this information is just as valuable.
B - Proposing the organ donation option/unknown wishes
If the patient had not made his or her wishes regarding organ donation known, ask the family to respond based on the potential donor’s values—sharing, social solidarity, helping others and generosity.
In this situation, one key phrase is often used: “If your (brother, wife, mother, son, etc.) could speak right now, knowing what we know, would (he/she) be in favour of organ donation?”
Organ donation as an end-of-life option can be a source of comfort for grieving families. It can also give them the feeling that they are helping people awaiting this precious gift.
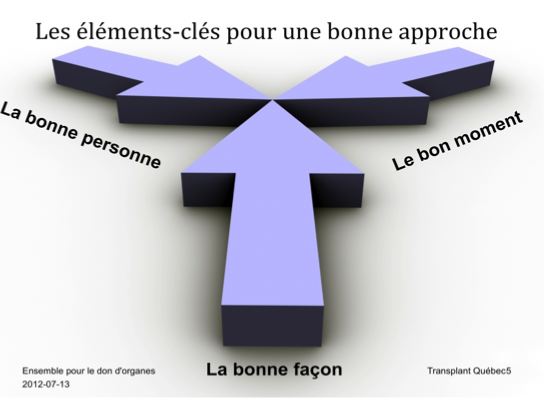
The best practices developed in conjunction with hospitals focus on three important factors that need to be considered when proposing the organ donation option to families.
1. The right time
a) Once the family understands that the patient will not survive
b) When the family initiates the discussion about organ donation
c) When the decision is made to withdraw life-sustaining treatment
2. The right person
The donation option is presented by the treatment team member (physician, nurse, spiritual advisor, social worker) who has the best relationship with the patient’s family or the most experience and skill in communicating with families.
3. The right approach
The decoupling approach, used in a private setting and the appropriate surroundings, in combination with attentiveness and the appropriate language.
Once the organ donation option has been proposed, give the family time to reflect. Be attentive and answer their questions.
Then, once the family has agreed (at least orally), Transplant Québec’s clinical coordinator/advisor will arrive to take the next steps.
In a case where the family refuses, verify their reason to make sure that it does not derive from a lack of understanding, taboo or myth. Examples:
- The family members do not understand what brain death means and they are hoping for recovery.
- They think their loved one’s medical history makes him or her an unsuitable candidate for donation.
- They believe that their religion forbids organ donation.
- They are afraid that the body will be returned to them mutilated.
Tell the family that they can speak with Transplant Québec’s coordinator/advisor or your institution’s nurse consultant in organ donation and care partnerships/resource nurse should they have any questions.
In the event that the family makes a free and informed decision to decline the offer, it is essential to respect their decision and continue supporting them until the end.
